INFORMATION
Why is turbinate reduction done?
Most people experience issues with their turbinates from time to time. These problems, and the breathing difficulties that accompany them, usually go away on their own or with medical treatment.
Some common and reversible causes of turbinate enlargement include:
- allergies
- infections
- weather changes
- stress
- medications
- hormonal changes
But there are some causes of turbinate enlargement or displacement that can’t easily be reversed and may require turbinate reduction. These include:
- chronic infections
- severe allergies
- anatomic issues with the nose
Turbinate reduction is also commonly recommended for those who undergo septoplasty, which is surgery to correct a deviated septum.
A deviated septum is a shift of the bone and cartilage between the nose’s two nostrils. It can cause compression of the turbinates and trouble breathing.
A turbinate reduction can help further open up the airways of a person who’s had a septoplasty.
What happens during the procedure?
There are several ways to reduce the size of the turbinates. Some are less invasive than others.
CAUTERIZATION, COBLATION, AND RADIOFREQUENCY REDUCTION
In some cases, doctors recommend surgeries that shrink the turbinate’s without removing any underlying bone or tissue.
To do this, a surgeon uses a special needle-like device that heats the turbinate’s using a heat source or energy waves. This causes scar tissue to form, reducing the turbinate’s size.
These procedures fall under the categories of cauterization, coblation, and radiofrequency reduction.
They usually take about 10 minutes and can be performed under local anesthesia in a surgeon’s office. Local anesthesia is injected into the nasal tissues using a needle.
Usually no special preparation is needed. These procedures are often used in less severe cases of turbinate enlargement.
Surgical removal
In other cases, a doctor may recommend that parts of the turbinates be surgically removed. These procedures are usually done in an operating room under general anesthesia using a gas that you inhale or with an anesthetic given intravenously (through an IV).
You shouldn’t eat or drink beforehand, usually starting the night before. You should also avoid taking medications containing aspirin or ibuprofen for two weeks before surgery to minimize the risk of bleeding.
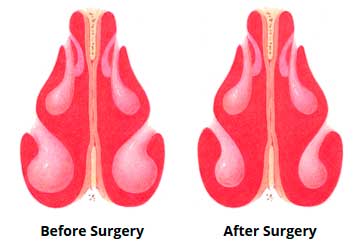
During this kind of turbinate reduction, a surgeon cuts into the turbinates to remove some of the bone beneath them, to reduce their overall size.
They may also use a small handheld device that can shave away some of the tissue around your turbinates, further opening your nasal cavity.
Surgical removal of underlying bone or tissue surrounding the turbinates is usually reserved for more serious cases of turbinate enlargement. It’s often done during a septoplasty.
A septoplasty also involves cutting into the nasal cavity to correct a deviated septum.
What’s recovery like?
Recovery times vary for each type of turbinate reduction procedure. For less invasive turbinate reductions, recovery is usually quick and not very painful. In about three weeks, the new scar tissue in your nose should be completely healed.
For the more invasive type of turbinate reduction surgery, recovery takes three to six months. For up to a week after surgery, you may need to pack your nostrils with gauze to keep tissues in place. Over time, your nasal tissues will heal into place.
To avoid possible bleeding and swelling, avoid strenuous activities and blowing your nose for several weeks after your surgery.
Your doctor may also recommend you elevate your head while sleeping and wear clothing that fastens in front — rather than clothing that is pulled over your head — to avoid irritating your nose.
What’s the outlook?
The goal of turbinate reduction surgery is to shrink the size of the turbinates without removing too much tissue.
A lack of turbinate tissue may cause the nasal cavity to become very dry and crusty. In some cases, a reduced turbinate may regrow, requiring a repeat surgery to reduce their size.
In most cases, turbinate reductions are successful at opening the airways and making breathing easier. By following your surgeon’s pre-operative and after-care instructions, you can speed your healing and maximize your results.
Your Recovery
You may have a drip pad under your nose to collect mucus and blood. Change it only when it bleeds through. You may have to do this every hour for 24 hours after surgery.
You may have some swelling of your nose, upper lip, cheeks, or around your eyes. You may have some bruises around your nose and eyes. Your nose may be sore and will bleed. You may feel “stuffed up” as though you have a bad head cold. This will last for several days after surgery.
The tip of your nose and your upper lip and gums may be numb. Feeling will return in a few weeks to a few months. Your sense of smell may not be as good after surgery. It will likely return to normal in 1 to 2 months.
Most people can return to work or school in about 1 week and to their normal routine in about 3 weeks. However, this varies with your job and the extent of your surgery. You will probably feel fully recovered in 1 to 2 months.
You may need to visit your doctor regularly for 3 to 4 months after your surgery. Your doctor will check to see that your nose is healing well.
This care sheet gives you a general idea about how long it will take for you to recover. But each person recovers at a different pace. Follow the steps below to get better as quickly as possible.
Other instructions
- Do not blow your nose for 1 week after surgery, or until your doctor says it is okay.
- Do not put anything into your nose.
- If you must sneeze, open your mouth and sneeze naturally.
- Keep your mouth clean. Rinse your mouth with salt water or a nonalcohol mouthwash after each meal and before bedtime.
- After any packing is removed, use saline (saltwater) nasal washes to help keep your nasal passages open and wash out mucus and bacteria. You can buy saline nose drops at a grocery store or drugstore. Or you can make your own at home by adding 1 teaspoon of salt and 1 teaspoon of baking soda to 2 cups of distilled water. If you make your own, fill a bulb syringe with the solution, insert the tip into your nostril, and squeeze gently. Blow your nose.
- You can wear your glasses when you wish. Do not wear contacts until the day after the surgery.
- Do not travel by airplane for at least 2 weeks. Your sinuses are still healing, and the changes in air pressure can affect them.
Call your doctor if:
- You have bleeding through the nasal packing that is not slowing.
- You have symptoms of infection, such as:
Increased pain, swelling, warmth, or redness.
- Red streaks coming from the area.
- Pus draining from the area.
- A fever.
- You have new pain, or your pain gets worse.
Is turbinate surgery painful?
congestion, nasal discharge, and headache, for 1 – 2 weeks after turbinate surgery. Pain is usually mild; prescription pain medications may be needed for a few days after the surgery. A prescription will be given at the time of surgery.
How do I clean my nose after turbinate surgery?
- Use salt water (saline) rinses beginning 1 to 2 days after surgery to wash away any crust and surgical debris. …
- Your doctor may recommend that you use a nasal steroid spray 15-30 minutes after using the salt-water rinse.
- You will need several visits after surgery to clear out old blood and mucus.





