INFORMATION
Anterior vaginal wall repair
Anterior vaginal wall repair is a surgical procedure. This surgery tightens the front (anterior) wall of the vagina.
Description
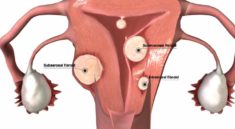
The anterior vaginal wall can sink (prolapse) or bulge. This occurs when the bladder or the urethra sink into the vagina.
The repair may be done while you are under:
- General Anesthesia: You will be asleep and unable to feel pain.
- Spinal anesthesia: You will be awake, but you will be numb from the waist down and you will not feel pain. You will be given medicines to help you relax.
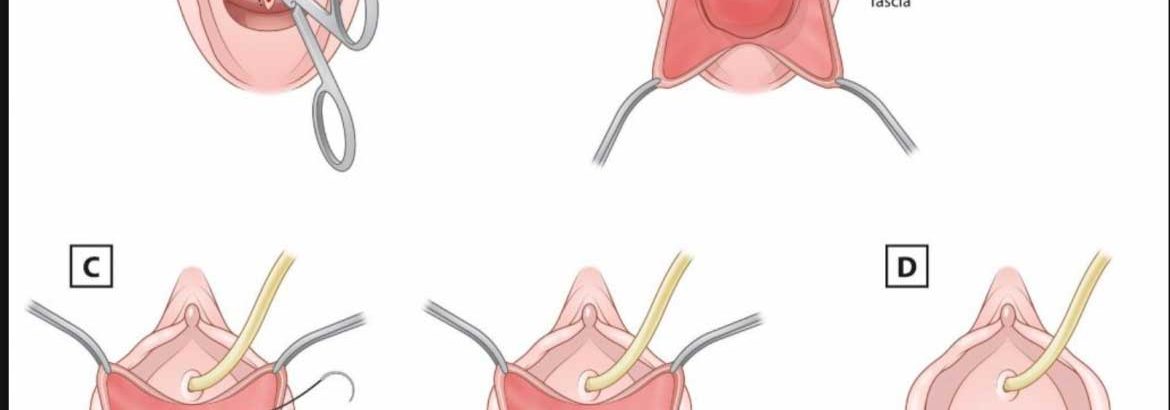
Your surgeon will:
- Make a surgical cut through the front wall of your vagina.
- Move your bladder back to its normal location.
- May fold your vagina or cut away part of it.
- Put sutures (stitches) in the tissue between your vagina and bladder. These will hold the walls of your vagina in the correct position.
- Place a patch between your bladder and vagina. This patch can be made of man-made material (synthetic skin) or commercially available biological material (such as pig or cow skin or cadaveric tissue).
- Attach sutures to the walls of the vagina to the tissue on the side of your pelvis.
Sometimes, the surgeon will also make a surgical cut in your belly. This cut may be up and down or across.
Why the Procedure is Performed
This procedure is used to repair sinking or bulging of the vaginal wall.
Symptoms of anterior vaginal wall prolapse include:
- You may not be able to empty your bladder completely.
- Your bladder may feel full all the time.
- You may feel pressure in your vagina.
- You may be able to feel or see a bulging at the opening of the vagina.
- You may have pain when you have sex.
- You may leak urine when you cough, sneeze, or lift something.
- You may get bladder infections.
This surgery by itself does not treat stress incontinence. Stress incontinence is the leaking of urine when you cough, sneeze, or lift. It may be performed along with other surgeries.
Before doing this surgery, your doctor may have you:
- Learn pelvic floor muscle exercises (Kegel exercises)
- Use estrogen cream in your vagina
- Try a device called a pessary in your vagina to hold up the prolapse
Before the Procedure
Always tell your provider what drugs you are taking. Also tell the provider about the drugs, supplements, or herbs you bought without a prescription.
During the days before the surgery:
- You may be asked to stop taking aspirin, ibuprofen (Advil, Motrin), warfarin (Coumadin), and any other drugs that make it hard for your blood to clot.
- Ask your provider which drugs you should still take on the day of your surgery.
On the day of your surgery:
- You very often will be asked not to drink or eat anything for 6 to 12 hours before the surgery.
- Take the medicines your provider told you to take with a small sip of water.
- Your provider will tell you when to arrive at the hospital.
After the Procedure
You may have a catheter to drain urine for 1 or 2 days after surgery.
You will be on a liquid diet right after surgery. When your normal bowel function returns, you can return to your regular diet.
You should not insert anything in the vagina or have sex until your surgeon says it is OK.
Outlook (Prognosis)
This surgery will very often repair the prolapse and the symptoms will go away. This improvement will often last for years.
Risks
Risks for anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots
- Infection
Risks for this procedure include:
- Damage to the urethra, bladder, or vagina
- Irritable bladder
- Changes in the vagina (prolapsed vagina)
- Urine leakage from the vagina or to the skin (fistula)
- Worsening urinary incontinence
- Lasting pain
- Complications from the material used during surgery (mesh/grafts)
How long does prolapse surgery take?
These catheters are usually only necessary for 3 to 7 days. Most patients require at least some prescription strength pain medicine for about one to two weeks after surgery. After any surgery to correct urinary incontinence or prolapse, we ask that patients “take it easy” usually for 12 weeks to allow proper healing.
When can I go back to work after prolapse surgery?
You may need about 4 to 6 weeks to fully recover from open surgery and 1 to 2 weeks to recover from laparoscopic surgery or vaginal surgery. It is important to avoid heavy lifting while you are recovering, so that your incision can heal.
When can I drive after prolapse surgery?
Also we advise you do not smoke as this increases the risk of a long term cough which has a very high risk of making the prolapse reoccur. You may drive once you can perform an emergency stop without this causing you pain. This is usually around six weeks after your operation.
When can I exercise after prolapse surgery?
The best time for you to return to exercise is something you’ll need to discuss with your surgeon during your postoperative visit approximately 6 weeks after your prolapse surgery. Some women receive approval to return to general exercise 6-8 weeks after prolapse surgery
What happens in prolapse surgery?
A procedure to prevent urinary incontinence may be done at the same time. Colporrhaphy—Used to treat prolapse of the anterior (front) wall of the vagina and prolapse of the posterior (back) wall of the vagina. … Surgical mesh is attached to the cervix and then to the sacrum, lifting the uterus back into place.
What is the best surgery for prolapsed bladder?
Laparoscopic pelvic reconstructive surgery can thus be used to repair bladder prolapse, uterine prolapse (with or without hysterectomy), vaginal prolapse and enteroceles.
Can a prolapse return after surgery?
Risk factors for the recurrence of pelvic organ prolapse after vaginal surgery: a review at 5 years after surgery. … Five years after surgery, 42 women (31.3%) presented anatomical recurrence of the prolapse (grade > or = II), and only 10 of the 134 (7.4%) had prolapse-related symptoms.
Can a prolapse make you feel tired?
Pelvic organ prolapse can produce varying degrees of discomfort and a variety of symptoms. The most common complaints are leg fatigue, low back pain, and a feeling of pelvic pressure, or bearing down. … Prolapse of the bladder, urethra, or uterus can cause stress urinary incontinence and difficulty starting to urinate.