INFORMATION
What is an abdominal myomectomy?
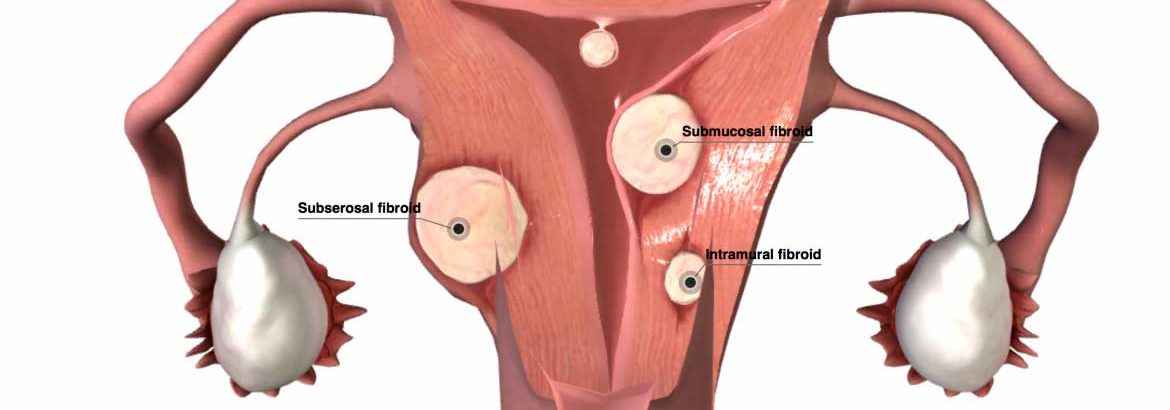
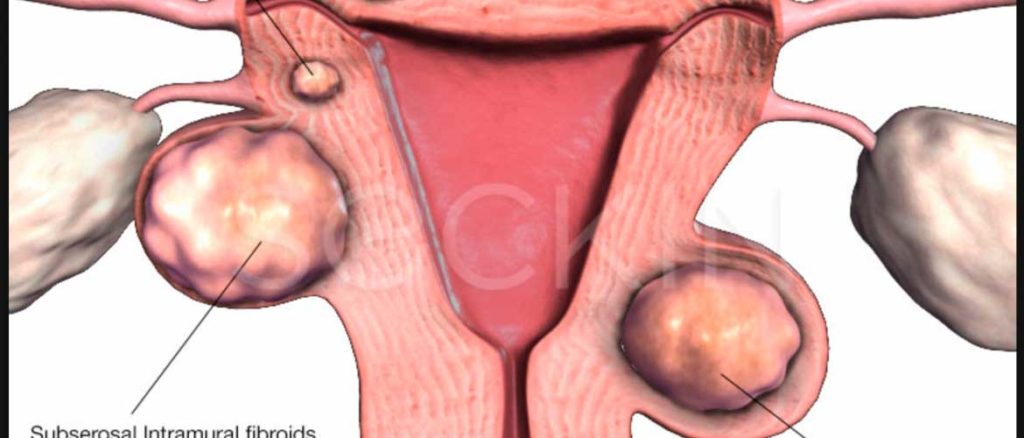
A myomectomy is surgery to remove fibroids from the uterus. Uterine fibroids are benign (non-cancerous) tumors of the uterine wall or muscle.
The surgery is done through a cut (incision) the doctor makes in your lower belly. In many cases, the doctor makes the incision just above the pubic hairline. In other cases, the incision runs from the belly button to the pubic hairline. Either incision leaves a scar, which usually fades with time.
Most women go home 1 to 4 days after the surgery. You can expect to feel better each day, but you will probably need about 4 to 6 weeks to fully recover.
This surgery should decrease the pain and heavy bleeding that are caused by fibroids. You will still have your uterus after the surgery. Having a myomectomy, unlike many other treatments for fibroids, means you probably will be able to have children. But some surgeries for large fibroids may damage the uterus. This can make a future pregnancy more difficult or risky. Talk to your doctor about this as you prepare for your surgery.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor or nurse call line if you are having problems. It’s also a good idea to know your test results and keep a list of the medicines you take.
What happens before surgery?
- It is important that you understand exactly what surgery is planned, the risks, benefits, and other options before your surgery.
- Tell your doctors ALL the medicines and natural health products you take. Some of these can increase the risk of bleeding or interact with anesthesia. Your doctor will tell you which medicines to take or stop before your surgery.
If you take blood thinners, such as warfarin (Coumadin), clopidogrel (Plavix), or aspirin, be sure to talk to your doctor. He or she will tell you if you should stop taking these medicines before your surgery. Make sure that you understand exactly what your doctor wants you to do.
You may need to stop taking certain medicines a week or more before surgery, so talk to your doctor as soon as you can.
You may need to take a laxative or enema before surgery. Your doctor will tell you how to do this.
TAKING CARE OF YOURSELF BEFORE SURGERY
- Build healthy habits into your life. Changes are best made several weeks before surgery, since your body may react to sudden changes in your habits.
Stay as active as you can.
Eat a healthy diet.
Cut back or quit alcohol and tobacco.
At the hospital or surgery center
A small tube (IV) will be placed in a vein, to give you fluids and medicine to help you relax. Because of the combination of medicines given to keep you comfortable, you may not remember much about the operating room.
You will be kept comfortable and safe by your anesthesia provider. The anesthesia may range from making you fully asleep, to simply numbing the area being worked on. This will depend on the procedure you are having, as well as a discussion between your doctor, the anesthesia provider, and you.
The surgery will take about 2 hours.
As you wake up in the recovery room, the nurse will check to be sure you are stable and comfortable. It is important for you to tell your doctor and nurse how you feel and ask questions about any concerns you may have.
Going home
Be sure you have someone to drive you home.
For your safety, you should not drive until you are no longer taking pain medicines and you can move and react easily.
Arrange for extra help at home after surgery, especially if you live alone or provide care for another person.
Your Recovery
You can expect to feel better and stronger each day, although you may tire quickly and need pain medicine for a week or two. You may need about 4 to 6 weeks to fully recover.
Do not lift anything heavy while you are recovering so that your incision and your belly muscles can heal.
How can you care for yourself at home?
- Rest when you feel tired. Getting enough sleep will help you recover.
- Try to walk each day. Start out by walking a little more than you did the day before. Bit by bit, increase the amount you walk. Walking boosts blood flow and helps prevent pneumonia and constipation.
- For 4 to 6 weeks, avoid lifting anything that would make you strain. This may include a child, heavy grocery bags and milk containers, a heavy briefcase or backpack, cat litter or dog food bags, or a vacuum cleaner.
- Avoid strenuous activities, such as biking, jogging, weightlifting, and aerobic exercise, for 4 to 6 weeks.
- You may shower. Pat the incision dry when you are done. Do not take a bath for the first week after surgery or until your doctor tells you it is okay.
- You may have some light vaginal bleeding. Wear sanitary pads if needed. Do not douche or use tampons.
- Ask your doctor when you can drive again.
- You will probably need to take 2 to 4 weeks off work. It depends on the type of work you do and how you feel.
- Do not have sex until your doctor tells you it is okay.
- Talk about birth control with your doctor. Do not try to become pregnant until your doctor says it is okay.
Diet
- You can eat your normal diet. If your stomach is upset, try bland, low-fat foods like plain rice, broiled chicken, toast, and yogurt.
- Drink plenty of fluids (unless your doctor tells you not to).
- You may notice that your bowel movements are not regular right after your surgery. This is common. Try to avoid constipation and straining with bowel movements. You may want to take a fibre supplement every day. If you have not had a bowel movement after a couple of days, ask your doctor about taking a mild laxative.
Medicines
- Your doctor will tell you if and when you can restart your medicines. He or she will also give you instructions about taking any new medicines.
- Take pain medicines exactly as directed.
If you are not taking a prescription pain medicine, take an over-the-counter medicine such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin), or naproxen (Aleve). Read and follow all instructions on the label.
Do not take two or more pain medicines at the same time unless the doctor told you to. Many pain medicines contain acetaminophen, which is Tylenol. Too much acetaminophen (Tylenol) can be harmful.
- If you think your pain medicine is making you sick to your stomach:
Take your medicine after meals (unless your doctor tells you not to).
Ask your doctor for a different pain medicine.
- If your doctor prescribed antibiotics, take them as directed. Do not stop taking them just because you feel better. You need to take the full course of antibiotics.
Incision care
- If you have strips of tape on the cut (incision) the doctor made, leave the tape on for a week or until it falls off.
- Wash the area daily with warm, soapy water and pat it dry.
- Keep the area clean and dry. You may cover it with a gauze bandage if it weeps or rubs against clothing. Change the bandage every day.
Call your doctor or nurse call line now if :
- You have pain that does not get better after you take pain medicine.
- You cannot pass stool or gas.
- You have vaginal discharge that has increased in amount or smells bad.
- You are sick to your stomach or cannot drink fluids.
- You have loose stitches, or your incision comes open.
- Bright red blood has soaked through the bandage over your incision.
- You have signs of infection, such as:
Increased pain, swelling, warmth, or redness.
Red streaks leading from the incision.
Pus draining from the incision.
A fever.
- You have bright red vaginal bleeding that soaks one or more pads in an hour, or you have large clots.
- You have signs of a blood clot in your leg (called a deep vein thrombosis), such as:
Pain in your calf, back of the knee, thigh, or groin.
Redness and swelling in your leg or groin.
Watch closely for any changes in your health and be sure to contact your doctor or nurse call line if you have any problems.