INFORMATION
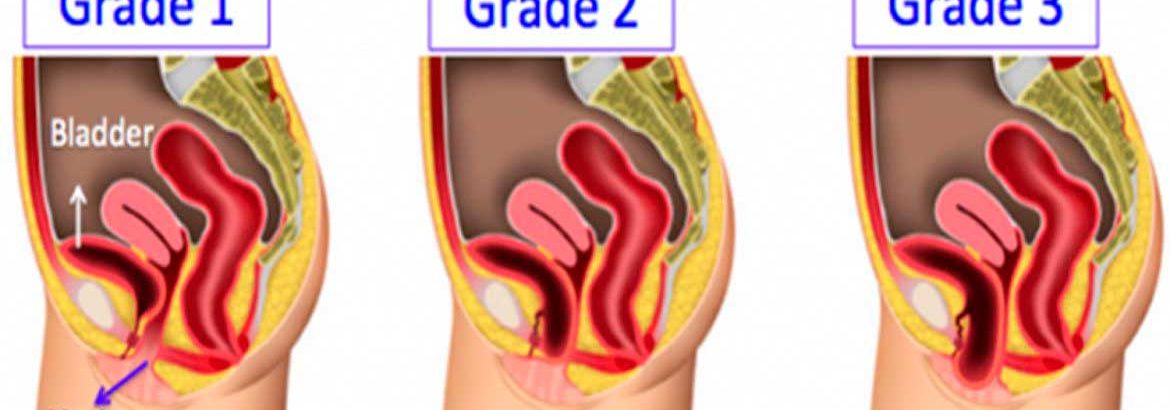
A cystocele is when part of the bladder wall bulges into the vagina. The bulge happens through a defect in the wall between the bladder and vagina.
A rectocele is when part of the wall of the rectum bulges into the vagina. The bulge happens through a defect in the wall between the rectum and vagina.
Reasons for Procedure
Cystocele and rectocele can cause problems going to the bathroom such as frequent urination, urine leakage, and difficulty urinating. Pain during sex may also occur. This surgery is done to help relieve these symptoms.
Most often, this type of surgery is not done until all other treatments have been tried. Other treatments may include muscle exercises and the insertion of a supportive device called a pessary. If you have tried these treatments and have had no relief, your doctor may suggest surgical repair.
What to Expect
PRIOR TO PROCEDURE
- Talk to your doctor about your current medications. Certain medications may need to be stopped before the procedure.
- Eat a light meal the evening before the surgery.
- Do not have anything to eat or drink after midnight on the night before the procedure.
- If you are having a rectocele repair, you may need to have an enema the night before the surgery.
Anesthesia
You will have either general anesthesia.
DESCRIPTION OF THE PROCEDURE
You may be given an antibiotic just before surgery. A tube called a catheter will be inserted in the urethra. This will allow urine to drain and decrease pressure on the bladder.
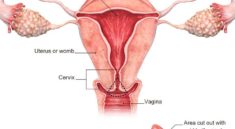
A cut will be made in the skin to expose the involved muscle and tissue. In some cases, the muscles and tissue will be sewn back onto itself. This will make it stronger. In other cases, a mesh-type material will be used to strengthen the tissue. Any tissue that has been weakened by previous surgeries, pregnancies, or age will be removed. Excess vaginal lining will be removed as well.
In some cases, a suspension or elevation procedure may be done. These are special sutures that provide extra support to the bladder.
How Long Will It Take?
45 minutes to 2 or more hours
How Much Will It Hurt?
You will likely experience vaginal discomfort for 1-2 weeks following the surgery. You will be given medication to help relieve this.
Average Hospital Stay
The usual length of stay is 1-2 days. Your doctor may choose to keep you longer if complications arise.
Possible Complications
Problems from the procedure are rare, but all procedures have some risk. Your doctor will review potential problems, like:
- Reaction to anesthesia
- Infection
- Bleeding
- Accidental damage to vagina, rectum, and bladder
- Accidental damage to nearby organs
- Difficulty with bowel movements
Before your procedure, talk to your doctor about ways to manage factors that may increase your risk of complications such as:
- Smoking
- Drinking
- Chronic disease such as diabetes or obesity
Prior pelvic surgery may increase the risk of complications.
Post-procedure Care
At the Hospital
- A medicated vaginal packing is usually left in the vagina overnight.
- If you had a rectocele repair, the bladder catheter will be removed as soon as you are able to use the bathroom on your own.
- If you had a cystocele repair, the bladder catheter often needs to stay in longer—sometimes 2-6 days. This will allow the bladder more time to begin to work normally.
- You may notice an odor and/or bloody discharge from the vagina for 1-2 weeks.
During your stay, the hospital staff will take steps to reduce your chance of infection such as:
- Keeping your incisions covered
- Washing your hands often and reminding visitors and healthcare providers to do the same
When you return home, do the following to help ensure a smooth recovery:
- Avoid lifting anything that weighs more than 10 pounds for about 6 weeks.
- Avoid sexual intercourse for about 6 weeks.
- Avoid inserting anything into the vagina, including tampons, for about 6 weeks.
Call Your Doctor
Contact your doctor if your recovery is not progressing as expected or you develop complications such as:
- Signs of infection, including fever and chills
- Excessive bleeding or any discharge from the incision site
- Unusually heavy vaginal bleeding or foul-smelling discharge from the vagina
- Nausea or vomiting
- Pain that you cannot control with the medications you have been given
- Inability to pass urine into the catheter
- Pain, burning, urgency or frequency of urination, or persistent blood in the urine
- Cough, shortness of breath, or chest pain
If you think you have an emergency, call for emergency medical services right away.
How long does prolapse surgery take?
These catheters are usually only necessary for 3 to 7 days. Most patients require at least some prescription strength pain medicine for about one to two weeks after surgery. After any surgery to correct urinary incontinence or prolapse, we ask that patients “take it easy” usually for 12 weeks to allow proper healing.
What happens in prolapse surgery?
A procedure to prevent urinary incontinence may be done at the same time. Colporrhaphy—Used to treat prolapse of the anterior (front) wall of the vagina and prolapse of the posterior (back) wall of the vagina. … Surgical mesh is attached to the cervix and then to the sacrum, lifting the uterus back into place.