INFORMATION
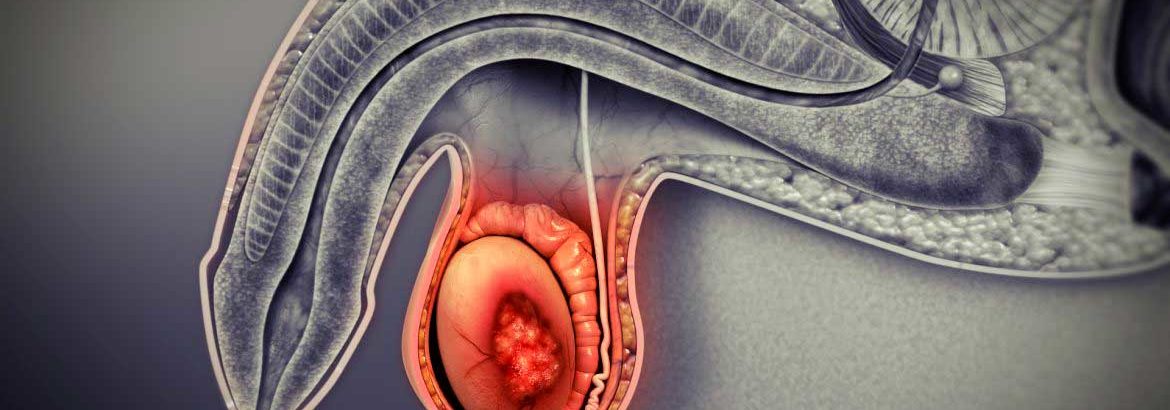
Surgical Procedures: Orchiectomy
What is an orchiectomy and how is it performed?
An orchiectomy is the removal of one or both testicles. The testicles rest below the penis in the scrotum. The testicles are glands that make sperm and testosterone.
An orchiectomy may be used to treat some cases of:
- Testicular and/or prostate cancer.
- Male breast cancer.
- Cancer prevention in men with an undescended testicle after puberty.
- Severe trauma.
- Male-to-female gender reassignment surgery.
There are different types of orchiectomy, including:
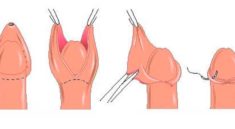
- Radical Inguinal Orchiectomy:The testicle and spermatic cord are removed through an incision made in the groin. At times, a prosthetic saline-filled testicular implant can be inserted.
- Simple Orchiectomy:During a simple orchiectomy, the testicle is removed through the scrotum. As in a radical inguinal orchiectomy, a prosthetic testicle can be inserted. In both simple and radical orchiectomy, a single testicle can be removed, or both testicles, which is called bilateral orchiectomy.
- Subcapsular Orchiectomy:During a subcapsular orchiectomy, the glandular tissue lining the testicles is removed, leaving the testicles in place.
What are the risks associated with an orchiectomy?
As with any surgery, there are risks and possible side effects. These can be:
- Reaction to anesthesia. (Anesthesia is the medication you are given to help you sleep through the surgery, not remember it and to manage pain. Reactions can include wheezing, rash, swelling and low blood pressure.)
- Blood clots.
- Loss of fertility.
- Erectile dysfunction.
- Loss of feeling in the groin and/or genitals.
- Low libido (sex drive).
- Hot flashes, mood swings, depression.
- Loss of muscle mass.
- Breast enlargement (gynecomastia).
- Weight gain.
- Change in self-image.
What is recovery like?
Recovery from an orchiectomy may include a short stay in the hospital, depending on the extent of the procedure you have had. You will be taught incisional care before being discharged from the hospital.
Your medical team will discuss with you the medications you will be taking (blood clot and infection prevention, pain management, nausea management, and constipation prevention.
Your DOCTOR will tell you what you should and should not do when you go home. This will often include:
- Wear a scrotal support and use ice packs as directed.
- Take pain medication as prescribed.
- Avoid straining with bowel movements and try to prevent constipation.
- Use a donut cushion when sitting for comfort.
- Do not lift anything heavy until instructed by your provider.
- No sports, jogging or running until you are told it is safe to do so.
Driving, resuming sexual activity and returning to work should be discussed with your healthcare team.
What will I need at home?
- Thermometer to check for fever, which can be a sign of infection.
- Ice packs.
- Scrotal support, such as a jock strap.
When do I call my doctor?
- Your team will tell you at what temperature they should be contacted.
- Groin redness and/or swelling.
- Swelling in the scrotum.
- Drainage and/or bleeding at the incision.
- Not being able to urinate.
How can I care for myself?
You may need a family member or friend to help you with your daily tasks until you are feeling better. It may take some time before your team tells you that it is ok to go back to your normal activity.
Be sure to take your prescribed medications as directed to prevent pain, infection and/or constipation. Call your team with any new or worsening symptoms.
There are ways to manage constipation after your surgery. You can change your diet, drink more fluids, and take over-the-counter medications. Talk with your care team before taking any medications for constipation.
Taking deep breaths and resting can help manage pain, keep your lungs healthy after anesthesia, and promote good drainage of lymphatic fluid. Try to do deep breathing and relaxation exercises a few times a day in the first week, or when you notice you are extra tense.
How long does it take to recover from having a testicle removed?
Most men are able to return to work or their normal activities in about 2 to 3 weeks after surgery.
How long does it take to recover from orchiectomy?
It can take two weeks to two months to fully recover from an orchiectomy. Don’t lift anything over 10 pounds for the first two weeks or have sex until the incision has fully healed. Avoid exercise, sports, and running for four weeks after surgery.
What are the side effects of having a testicle removed?
You will have some soreness and bruising for a couple of weeks after your operation. There are no lasting side effects after you have one testicle removed. Having one testicle removed won’t affect your ability to get an erection. For most men it won’t affect their ability to have children.
What happens after a testicle is removed?
When one testicle is removed, there is usually no effect on a man’s sexual function. Most of the time, the remaining testicle produces enough testosterone and sperm to compensate for the testicle that has been removed. Therefore, the man should still be able to get an erection and ejaculate as he did before.
How long does orchiectomy surgery take?
about 30 minutes
The first two types are usually done under local or epidural anesthesia and take about 30 minutes to perform. An inguinal orchiectomy is sometimes done under general anesthesia, and takes from 30 minutes to an hour to complete
Can testicular cancer be cured if it has spread?
If these tests do not find any signs that cancer has spread beyond the testicle, no other treatment is needed. … The cancer will come back in about 15% to 20% of patients, most often as spread to lymph nodes , but if it does, radiation or chemo can still usually cure the cancer