INFORMATION
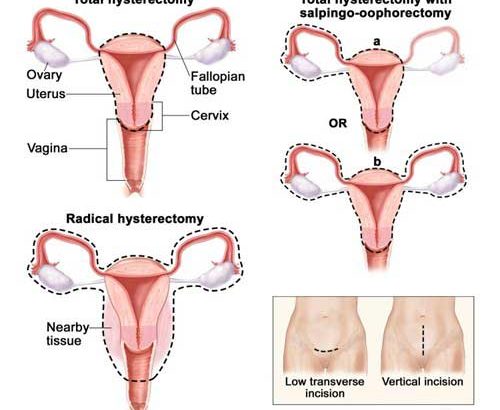
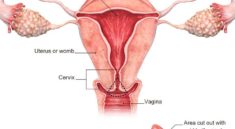
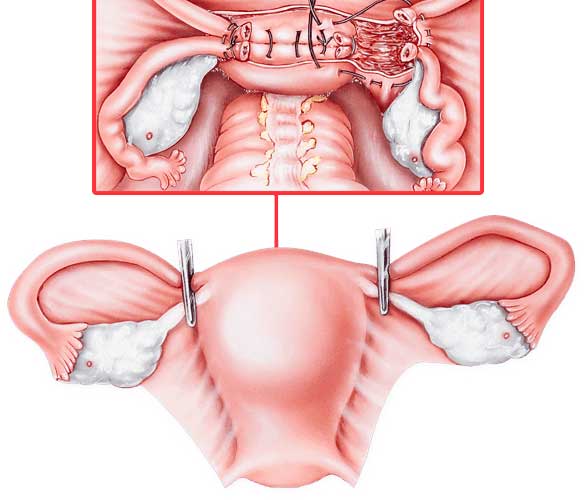
An abdominal hysterectomy is a surgical procedure that removes your uterus through an incision in your lower abdomen. Your uterus — or womb — is where a baby grows if you’re pregnant. A partial hysterectomy removes just the uterus, leaving the cervix intact. A total hysterectomy removes the uterus and the cervix.
Sometimes a hysterectomy includes removal of one or both ovaries and fallopian tubes, a procedure called a total hysterectomy with salpingo-oophorectomy.
Why it’s done
- Gynecologic cancer If you have a gynecologic cancer — such as cancer of the uterus or cervix — a hysterectomy may be your best treatment option.
- A hysterectomy is the only certain, permanent solution for fibroids — benign uterine tumors that often cause persistent bleeding, anemia, pelvic pain or bladder pressure.
- In endometriosis, the tissue lining the inside of your uterus (endometrium) grows outside the uterus on your ovaries, fallopian tubes, or other pelvic or abdominal organs. When medication or conservative surgery doesn’t improve endometriosis, you might need a hysterectomy along with removal of your ovaries and fallopian tubes (bilateral salpingo-oophorectomy).
- Uterine prolapse. Descent of the uterus into your vagina can happen when supporting ligaments and tissues weaken. Uterine prolapse can lead to urinary incontinence, pelvic pressure or difficulty with bowel movements.
- Abnormal vaginal bleeding. If your periods are heavy, irregular or prolonged each cycle, a hysterectomy may bring relief when the bleeding can’t be controlled by other methods.
- Chronic pelvic pain.
During hysterectomy surgery, your surgeon might also perform a related procedure that removes both of your ovaries and your fallopian tubes (bilateral salpingo-oophorectomy). You and your doctor should discuss ahead of time whether you need this procedure, which results in what’s known as surgical menopause.
With surgical menopause, menopause symptoms often begin suddenly for women after having the procedure done. Depending on how much these symptoms affect your quality of life, you may need short-term treatment with hormones.
Risks
A hysterectomy is generally very safe, but with any major surgery comes the risk of complications.
Risks associated with an abdominal hysterectomy include:
- Blood clots
- Infection
- Excessive bleeding
- Adverse reaction to anesthesia
- Damage to your urinary tract, bladder, rectum or other pelvic structures during surgery, which may require further surgical repair
- Earlier onset of menopause even if the ovaries aren’t removed
- Rarely, death
Before the procedure
Before surgery, you may have tests done to check for cancer, which could change your surgeon’s approach to surgery. Tests may include:
- Cervical cytology (Pap test),which detects the presence of abnormal cervical cells or cervical cancer
- Endometrial biopsy,which detects abnormal cells in the uterine lining or endometrial cancer
- Pelvic ultrasound,which may show the size of uterine fibroids, endometrial polyps or ovarian cysts
The day before and morning of your surgery, you will be instructed to shower using soap provided by your surgeon to reduce your risk of infection. A preoperative cleansing of your vagina (vaginal douche) or preoperative cleansing of your rectum (enema) also may be done. Immediately before surgery, you’ll receive an intravenous antibiotic medication to minimize your risk of infection after the procedure.
After the procedure
After surgery, you’ll remain in the recovery room for a few hours. Your health care team will:
- Monitor you for signs of pain
- Give you medicine for pain and to prevent infection
- Encourage you to get up and walk around soon after surgery
An abdominal hysterectomy usually requires a hospital stay of one to two days, but it could be longer. You’ll need to use sanitary pads for vaginal bleeding and discharge. It’s normal to have bloody vaginal drainage for several days to weeks after a hysterectomy. However, let your surgeon know if you have bleeding that’s as heavy as a menstrual period or bleeding that’s persistent.
The abdominal incision will gradually heal, but a visible scar on your abdomen will remain.
Your Recovery
You can expect to feel better and stronger each day, although you may need pain medicine for a week or two. You may get tired easily or have less energy than usual. This may last for several weeks after surgery. You will probably notice that your belly is swollen and puffy. This is common. The swelling will take several weeks to go down. It may take about 4 to 6 weeks to fully recover.
It is important to avoid lifting while you are recovering so that you can heal.
How can you care for yourself at home?
ACTIVITY
- Rest when you feel tired. Getting enough sleep will help you recover.
- Try to walk each day. Start by walking a little more than you did the day before. Bit by bit, increase the amount you walk. Walking boosts blood flow and helps prevent pneumonia and constipation.
- Avoid lifting anything that would make you strain. This may include a child, heavy grocery bags and milk containers, a heavy briefcase or backpack, cat litter or dog food bags, or a vacuum cleaner.
- Avoid strenuous activities, such as biking, jogging, weight lifting, or aerobic exercise, until your doctor says it is okay.
- You may shower. Pat the cut (incision) dry.
- Ask your doctor when you can drive again.
- You will probably need to take 2 to 4 weeks off from work. It depends on the type of work you do and how you feel.
- Your doctor will tell you when you can have sex again.
DIET
- You can eat your normal diet. If your stomach is upset, try bland, low-fat foods like plain rice, broiled chicken, toast, and yogurt.
- Drink plenty of fluids (unless your doctor tells you not to).
- You may notice that your bowel movements are not regular right after your surgery. This is common. Try to avoid constipation and straining with bowel movements. You may want to take a fibre supplement every day. If you have not had a bowel movement after a couple of days, ask your doctor about taking a mild laxative.
INCISION CARE
- If you have strips of tape on the cut (incision) the doctor made, leave the tape on for a week or until it falls off. Or follow your doctor’s instructions for removing the tape.
- Wash the area daily with warm, soapy water, and pat it dry. Don’t use hydrogen peroxide or alcohol, which can slow healing. You may cover the area with a gauze bandage if it weeps or rubs against clothing. Change the bandage every day.
- Keep the area clean and dry.
OTHER INSTRUCTIONS
- You may have some light vaginal bleeding. Wear sanitary pads if needed. Do not douche or use tampons.
Follow-up care is a key part of your treatment and safety.Be sure to make and go to all appointments, and call your doctor or nurse call line if you are having problems. It’s also a good idea to know your test results and keep a list of the medicines you take.
Call your doctor if:
- You have pain that does not get better after you take pain medicine.
- You cannot pass stools or gas.
- You have vaginal discharge that has increased in amount or smells bad.
- You are sick to your stomach or cannot drink fluids.
- You have loose stitches, or your incision comes open.
- Bright red blood has soaked through the bandage over your incision.
- You have signs of infection, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the incision.
- Pus draining from the incision.
- A fever.
- You have bright red vaginal bleeding that soaks one or more pads in an hour, or you have large clots.
- You have signs of a blood clot in your leg (called a deep vein thrombosis), such as:
- Pain in your calf, back of the knee, thigh, or groin.
- Redness and swelling in your leg.